What does a transdermal patch need to succeed?
Transdermal patches provide a convenient way to deliver medicine to patients consistently with little disruption to their routines. A successful, functional transdermal patch will effectively deliver medication over an intended period.
Yet, as products, they can be complex to design and produce due to many considerations, which is why many businesses turn to flexible material converters like Strouse, who has experience in helping optimize designs for both manufacturability and functionality.
The further you get in your transdermal patch design phase, the more you’ll notice certain factors that can make or break your product. To help you avoid unnecessary mistakes, we will examine the factors that can impact transdermal patch delivery systems.
Elements that Affect a Transdermal Patch’s Ability to Administer Medicine
If you’re familiar with designing transdermal patches, you may have discovered that manufacturing them can be a bit of a challenge.
One of the most considerable difficulties is ensuring that the drug contained within the patch gets administered to the patient as prescribed. If the patch isn’t designed and constructed to medicate the patient properly via the skin, it can be defective and potentially dangerous.
As you look through all the elements that can affect transdermal patch performance, consider how you might prepare for any potential pitfalls.
1. THE PATIENT
Let’s start with where the patch is going — on a living, breathing, and complex human being. The transdermal patch is applied directly to the skin, so the individual patient’s biology can seriously affect how the medicine is delivered.
Skin is alive, and different factors — such as the person’s age and skin hydration — play a role in the skin’s thickness and other characteristics. Those conditions can help or hurt how well the medicine is absorbed. All developers of transdermal patches must account for different skin types and biological components when creating each piece of the patch.
2. SHELF LIFE
Adhesive shelf life can be vital to product performance. Before a transdermal patch is placed on a patient, it will be sitting in storage for some time. The question is, how long will it sit in storage? Three months? Six? And once it’s off the shelf, how long until it’s opened and used?
One issue that could arise is the transdermal patch’s layers allowing the drug to be released before it’s used. These products are carefully designed to release medicine at a specific rate, and the amount of medicine retained will need to be accounted for and answered while the patch is still in development.
The medication’s release ultimately must be timed so that the patient receives the exact amount of the medicine they need at the right time, taking into account the entire lifespan of the patch.
3. ADHESIVE TYPE
A patch must be made with a suitable adhesive to allow the drug to pass through into the skin as needed while remaining attached for the specified time and not hurting the patient’s quality of life.
An adhesive could be comfortable and stay on the skin for the right amount of time, but it’s ineffective if it allows too much or too little of the drug into the skin.
Furthermore, if the adhesive is too strong, it could create discomfort for the patient while attached or when it’s removed. If it’s too weak, it might fall off early, before all the medicine has been delivered. Either of those situations with the wrong adhesive could significantly impact the treatment.
The chemistry of the adhesive must be just right so its interactions with the other elements of the patch and the patient’s skin aren't harmful.
4. BACKING LINER
Here’s something that might not be an obvious consideration: the backing liner.
When peeling off the backing liner to stick the patch to the skin, the liner must come off cleanly. If not, it risks pulling off too much of the adhesive, which could compromise it and release too much of the drug into the skin at once.
It could also mean that some medicine isn’t even there anymore. Recent designs have blended the active drug directly into the adhesive to make the patch more streamlined and less noticeable while worn. So, if a backing liner that’s too strong pulls away too much adhesive, the patch could lose some of its medical effectiveness.
The adhesive and backing liner must work perfectly in tandem to allow proper medication delivery.
5. OUTER LAYER
Transdermal patches tend to consist of multiple layers, meaning it’s also essential to consider the outer layer that will be directly exposed to clothing or the air itself.
If the outer layer isn’t properly constructed, the active ingredient could escape out that side rather than transfer through the adhesive layer. That’s going to cause underdosing issues and render the patch ineffective.
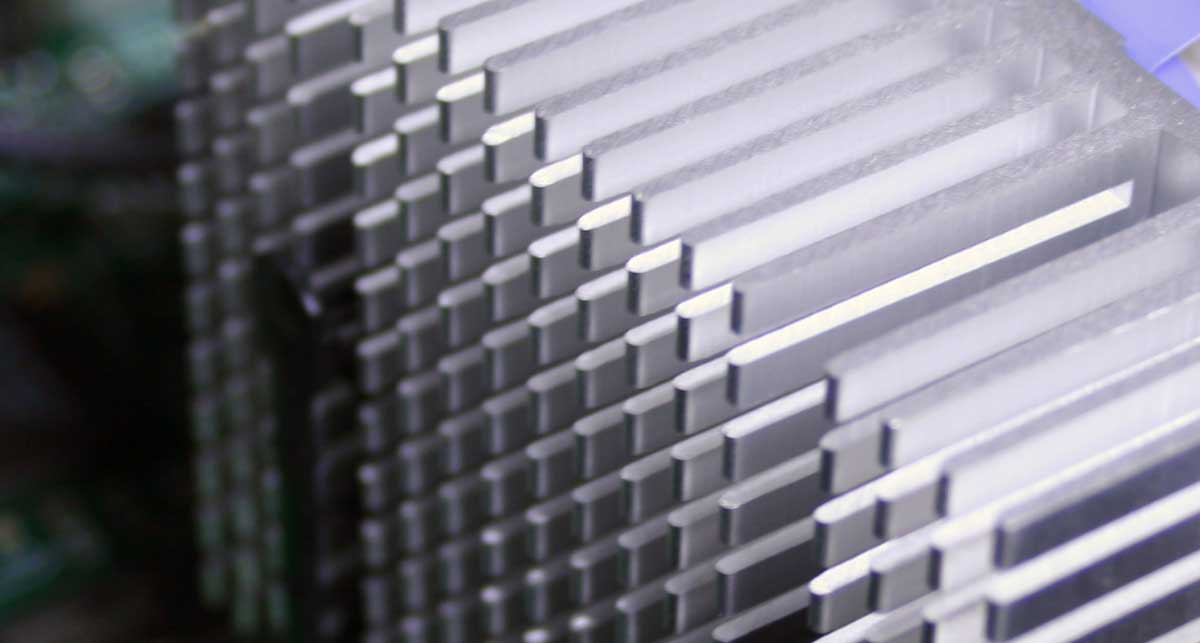
It’s vital that each layer, including the outer layer, be made with the tightest of tight tolerances to ensure the proper delivery of the medicine.
6. OVERALL PATCH SIZE
The overall patch size and thickness affect how much active drug it can contain. The bigger the patch, the more medicine you can fit!
It depends on the chemistry of the entire patch. If the patch is too thick or thin, medicine could be held up or released too quickly. If it’s too wide or too narrow, there could be too much or too little medicine inside from the get-go. A patch and its components — including the adhesive — must be cut and shaped to precise proportions.
Achieving a Smooth Production Process
The last thing you want is to let design and manufacturing complications come in between you and the many benefits of using transdermal adhesives. Instead, consider reaching out to the adhesive experts to find a solution for your product.
As we’ve advanced throughout the years, we’ve searched for ways to simplify the adhesive converting process without cutting a single corner in quality, safety, or efficacy. We’ve found a way to increase conversion speeds, improve accuracy and quality, and ensure cleanliness, all in a more efficient process.
Your product deserves a customized solution that will leave you with accurate and functional part components. Feel free to reach out and contact us if you’re interested, or check out more information about transdermal patch systems in our Learning Center.
Originally published: January 27, 2022